Cutting infection rate by half is not the same as protecting half the people from infection
Kaiser explains what 50% vaccine efficacy actually means, and it's not what you think.
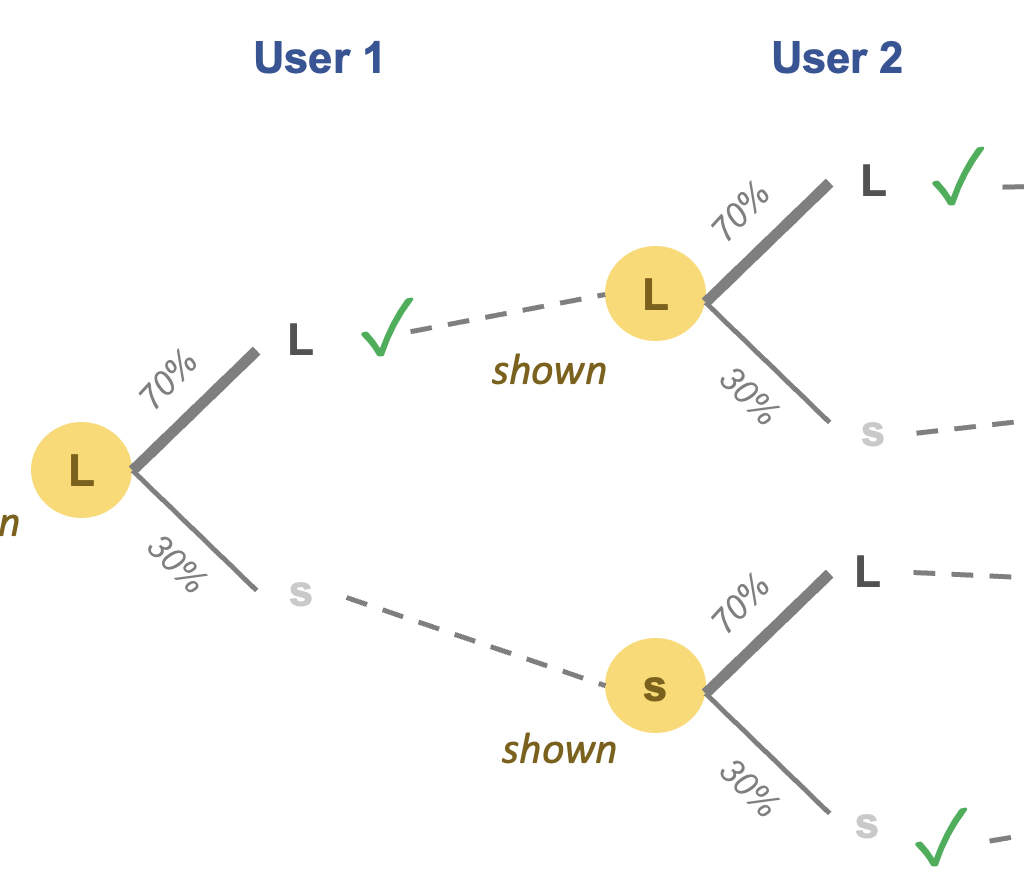
If you've read my previous post on "Masks and vaccines", you already know the answer.
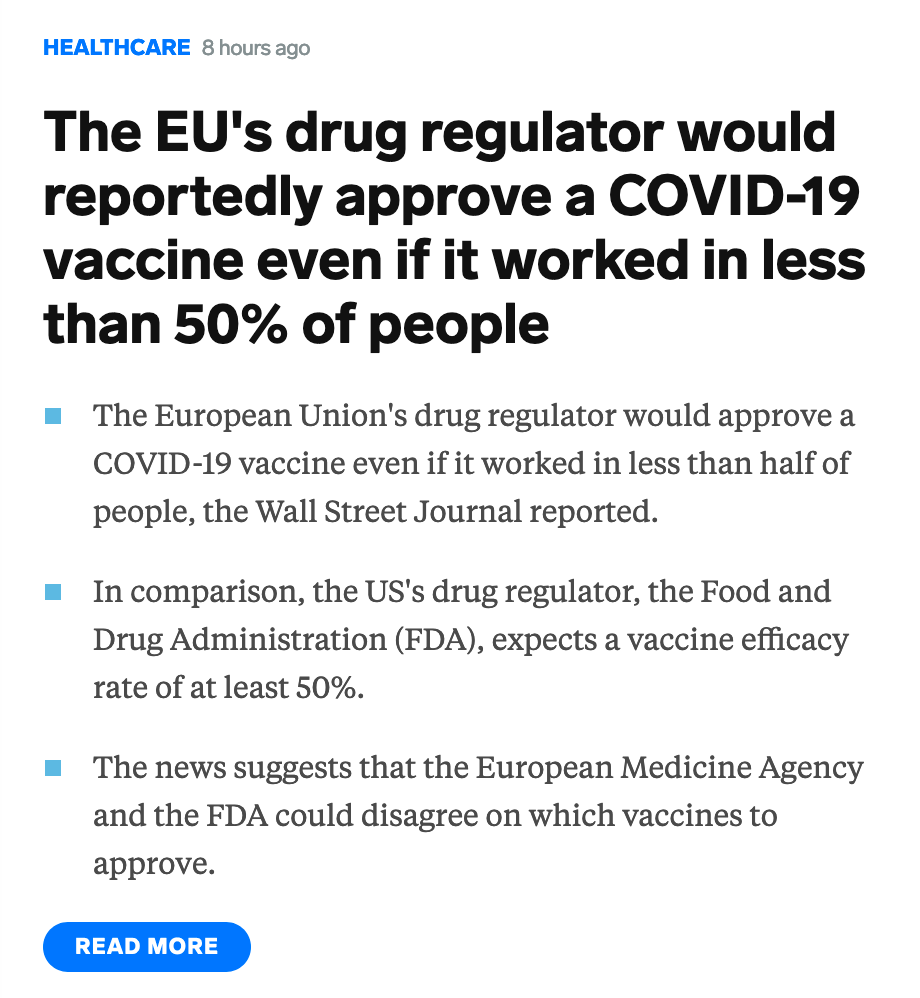
But some in the media have not gotten the message. Here is Business Insider's headline from last night:

The headline equates "50% vaccine efficacy" with "worked in 50% of people". If 1,000 people get vaccinated, 500 would be protected. By protection, I presume they mean people who would have gotten sick if not for the vaccine. [Note: biostatisticians use the term efficacy when the data come from the gold-standard randomized clinical trial while they use effectiveness when the data are observational.]
Presumably, the other 500 people would get infected despite getting vaccinated, and that's the opposite of "working". Think about how implausible this interpretation is. It makes a glorious assumption - that the baseline infection rate for the unvaccinated population is 100 percent. If the vaccine were not available, then all 1,000 would get infected.
***
That assumption is directly contradicted by information from the vaccine trials. My review of the Moderna trial documents revealed that the cumulative baseline rate of infection over a six-month period is (assumed to be) 0.75%. So, only 7 or 8 people out of 1,000 who got placebo during the trial are expected to get infected over six months. This puts a lid on how many people can actually benefit. A 100% efficacious vaccine would eliminate these 7 or 8 infections. A 50% efficacious vaccine would reduce infections by half, that is to say, 3 or 4 infections. Cutting the number of infections from 8 to 4 per 1,000 is still a good thing but it's not true that 500 people are protected.
Remember no one knows which 8 people would catch the virus. If we knew, we would just vaccinate them.
Cutting infection rate by half is not the same as protecting half the people from infection.
***
Regarding the 993 or 994 people who are not expected to catch the virus in the six-month period, regardless of whether they are vaccinated, one hopes that the vaccine gives them protection beyond the six months. If they don't get vaccinated, perhaps over time, they will catch it, and if they do, they won't.
I say "hope" because we have no idea if this scenario will play out. A real problem with the conversation around vaccine efficacy is ignoring the period of protection.
And the reason we cannot talk about the period of protection is because the period of observation in the vaccine trials is so short. Remember the FDA announced a rule requiring that the median participant in the vaccine trials must have been observed for two months. With such a rule, we can't even talk about six months of protection, let alone two years.
The math looks more appealing if we prolong the period of protection: let's assume that over a two-year period, 40% of an unvaccinated population will get infected. Now, if 1,000 people are vaccinated, and the vaccine is 50% efficacious over two years, then 200 infections will be avoided while 200 others will still get infected.
The longer the period of observation in the vaccine trials, the longer we can establish the period of protection, the greater the benefit of the vaccine. It's a delicate balancing act between getting a vaccine to market and getting one that confers a longer period of protection.